Laurie's Blogs.
May 2020
Reversing Osteoarthritis
This is a repurposed blog. I wrote this for https://caninearthritis.co.uk/, but I like it, and I've wanted to use if here for a while now. So here it is!
By Laurie Edge-Hughes, BScPT, MAnimSt (Animal Physio.), CAFCI, CCRT
Calgary, Alberta, Canada
Not too long ago, I received a request from a medical journal editor asking if I would like to contribute an article on the topic of ‘Can Osteoarthritis be Reversed?’. Now, before you get excited thinking that I might be an expert on that topic – I’m not – or that I have a protocol to make this happen – I don’t – it simply made me ponder the question! CAN osteoarthritis be reversed?
I’ve heard it said, “If my cells are turning over all the time, why do I keep getting the same old crappy knee?” Right! Why indeed? Bone cells turn over every 3 months, skin cells every 10 – 30 days, and your skeleton in general updates itself by 10% a year! (1) So, I decided to jump into the literature. I was directed to studies on stem cell (not about stem cell injections as a treatment, but rather your body’s innate stem cells) and how high cellular turnover seems to protect against aging, however if high cell turnover is in conjunction with cellular mutations, it might also hasten the development of cancer. (2) Hmm… well, we don’t want that either!
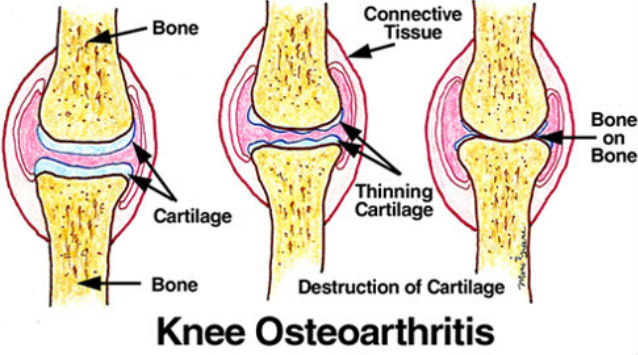
Then I came across a paper that made sense to me and seemed to address this topic nicely. I’ll summarize the abstract for you. Firstly, the author acknowledges that the reasons a joint might develop osteoarthritis (OA) is multifactorial. There might be mechanical damage (i.e. a torn ligament that leads to abnormal joint mechanics), or biochemical damage (i.e. inflammation in a joint leading to cartilage degeneration), or genetic (i.e. which could be a factor of conformation, like the unfortunate fact that I inherited my great grandmother’s turned in knees, or a dog that inherited hip dysplasia from a parent). The discussion then turns to chondrocytes (the cells that help to build and repair cartilage). In the early stages of OA, the body works like mad to try to repair damages, many different cells are sent to the area to deal with inflammation and tissue damage. However, the capacity of the adult articular chondrocyte to regenerate cartilage is limited, and the damage becomes irreversible unless the destructive process is interrupted. Thus, early diagnosis is of key importance, since therapies aimed at blocking or reversing cartilage damage will be more effective when there is the possibility of preserving normal homeostasis (i.e. The normal rate of cell destruction, restoration, and remodeling. This is the ‘turnover’ I was talking about earlier). At later stages, some different interventions may be required, such as tissue engineering in order to repair damaged cartilage. (3)
So, for the remainder of this article, I want to talk about preventing osteoarthritis before it begins. So, let’s say you know that your dog has hip or elbow dysplasia, or perhaps he injured his knee and had surgery (or not) for a cruciate ligament tear, or jumped off the bed and was limping and the vet told you that he hurt his shoulder or wrist. These are cases where you can become proactive in preventing osteoarthritis (as best you can)! You might also want to seek the guidance of a veterinary physiotherapist or rehab vet to help you address each goal.
Goal # 1: Manage the inflammation early. In a sudden onset trauma, inflammation is what signals the body to repair, but you don’t want the process to continue on for too long, otherwise it can do more harm than good. So, in the case of a joint injury (versus a muscle or tendon), I say, “Listen to your vet and put your dog on the anti-inflammatory now.” This doesn’t have to be a ‘forever-thing’, but a short-term use of non-steroidal anti-inflammatories is smart practice. This could be a good time for other tools such as laser therapy, acupuncture, or pulsed electromagnetic field (rehabilitation measures). Additionally, some rest is in order: Leash walks only, no playing, no sporting activities. If this is a genetic condition (i.e. hip or elbow dysplasia), this phase might be shorter than if this is a new trauma (i.e. a torn cruciate, or post-operative condition).
Goal # 2: Stimulate tissue healing. Here, you also have some of the rehabilitation tools that could work. Laser therapy, shockwave, and ultrasound all have an effect on tissue regeneration. Interestingly, there are some fascinating research papers that look at repairing damage to joints in cases where they ‘induced osteoarthritis in mice’ (i.e. in other words, the researchers made cuts to the cartilage in the mice joints so as to start an inflammatory and subsequent arthritic process). In many of those studies, they were able to significantly reduce the arthritic changes seen weeks and months later compared to the mice that didn’t receive therapies!
Goal # 3: Strengthen the surrounding muscles (after the inflammation has settled). Strengthening makes a huge impact on joint health. Strengthening helps cushion a joint by minimizing concussive forces (i.e. muscles can act as ‘shock absorbers’). Strengthening protects joints from the abnormal forces that can occur secondary to muscle weakness around a sore joint. Which exercises are best? Well, for one, it depends on which joint is affected, and secondly, you’ll want to be doing some specific muscle building exercises… not just walking. So, you’ll be looking for someone to prescribe them specifically for your dog’s injury.
Goal # 4: Maintain full joint range of motion. A joint gets its nutrition from lubricating all of its surfaces in synovial fluid (i.e. the fluid within the joint). So, if the outer edges of a joint don’t get lubricated, then that’s where the degenerative processes will begin. To stop this, your dog needs to be able to bend and straighten that joint fully. You might do this manually, or you can find an exercise that will accomplish this. For example, sitting square with knees, ankles, and hips tucked in is great in particular for knee or ankle arthritis. Lean on your veterinary physiotherapist or rehab vet for guidance here as well.
Goal # 5: Start the supplements now, and keep them on board forever. There are a number of supplements that aim to improve cartilage health. Vitamins, minerals, glycosaminoglycans, avocado-soybean unsaponifiable fractions, methylsulfonylmethane, s-adenosylmethionine, undenatured and hydrolyzed collagen preparations, phytoflavonoid compounds found in fruits, vegetables, spices, teas, and nuts, and other nutrients on the horizon. (4) This topic is very broad! Check the resources found here: https://caninearthritis.co.uk/managing-arthritis/diet-and-nutrition/available-supplements/
While I know that the information above is less useful to those of you with dogs suffering from more severe and painful versions of arthritis, this article might be of use to you for your younger dog, or your next dog, or the dog that is just going through something and you are curious about canine arthritis management proactively. So, to answer the original questions, ‘Can osteoarthritis be reversed?’ The answer is ‘Maybe… if you catch it in time!’
References:
1.http://book.bionumbers.org/how-quickly-do-different-cells-in-the-body-replace-themselves/ accessed April 15, 2019.
2.Wodarz D. Effect of stem cell turnover rates on protection against cancer and aging. J Theor Biol. 2007 Apr 7;245(3):449-58.
3.Goldring MB. Update on the biology of the chondrocyte and new approaches to treating cartilage diseases. Best Pract Res Clin Rheumatol. 2006 Oct;20(5):1003-25.
4.Lopez HL. Nutritional interventions to prevent and treat osteoarthritis. Part II: focus on micronutrients and supportive nutraceuticals. PM R. 2012 May;4(5 Suppl):S155-68.