Laurie's Blogs.
Dec 2023
Conservative Management of IVDH and Disc Resorption or Regression
From Khan S, et al. JSAP. 2022 Oct;63(10):797.
So my last blog received a comment that I think would be good to explore in this blog. (https://www.fourleg.com/Blog?b=650). The comment pertained to the following sentence in my last blog.
“‘…if human medicine utilizes foundational animal research to guide clinical treatments for people, why cannot human research be used to guide clinical treatments for animals?”
The comment was a response to the question posed, and it was:
1. There is a difference in weight bearing of the spine between dogs and humans.
2. There are differences between chondrodystrophic and non-chondrodystrophic breeds.
3. There are far more mineralized IVDD/IVDH cases than resorbed disc herniations in small animal veterinary medicine.
These are absolutely fair and valid points. So, I thought I would explore the research to look at spontaneous regression / resorption of canine discs. The compilation below is what I found – in chronologic order.
Hasegawa T, et al. The effect of age on inflammatory responses and nerve root injuries after lumbar disc herniation: an experimental study in a canine model. Spine (Phila Pa 1976). 2000 Apr 15;25(8):937-40. https://pubmed.ncbi.nlm.nih.gov/10767805/
There is an effect of age on the inflammatory response and nerve root injury caused by the herniated disc. Of beagles that were 6, 12, or 24 months of age, the 24-month-old cohort was the only group that demonstrated neovascularity, and intensive infiltration of lymphocytes, macrophages, and fibroblasts surrounding the nucleus pulposus fragment. Furthermore, degenerative changes of the nerve root fibers were observed in the 24-month-old group only.
As such the authors concluded that young animals possessed an apparent neuroprotective mechanism against inflammation or nerve degeneration (but not disc resorption), whereas the older animals with their apparent inflammatory response results in resorption of the nucleus pulposus fragment but can damage nerve root fibres.
Jensen VF. Asymptomatic radiographic disappearance of calcified intervertebral disc material in the Dachshund. Vet Radiol Ultrasound. 2001 Mar-Apr;42(2):141-8. https://pubmed.ncbi.nlm.nih.gov/11327362/
“The occurrence of asymptomatic disappearance of intervertebral disc calcification was evaluated in a radiographic prospective longitudinal study of 40 Dachshunds followed from 6 or 12 months of age to 2 years of age. Radiographic follow-up was performed at 3 to 4 years of age in 12 dogs. Disappearance of calcified disc material was observed in 9 thoracic and 1 lumbar intervertebral discs. The crude incidence rate tended to increase with age from 1 year of age. The features of the disappearing calcifications involved indicate that the phenomenon is part of the progressive degenerative process. A possible pathogenesis includes tearing of the annulus fibrosus due to the severe degeneration of the disc, followed by an inflammatory response to nuclear material and phagocytic resorption of calcified material.”
Shimizu J, et al. Inflammatory reaction in the herniated degenerative disc materials in miniature dachshunds. J Vet Med Sci. 2010 Jan;72(1):81-4. https://pubmed.ncbi.nlm.nih.gov/19915338/
“Histological and immunohistochemical studies were conducted using herniated intervertebral disc materials obtained surgically from 39 miniature dachshunds. Infiltration of inflammatory cells, such as macrophages, neutrophils, T or B lymphocytes, and multinucleated giant cells, were identified in intervertebral disc materials in 23 cases. Furthermore, proliferations of connective tissue, including neovascularization, were also observed in 17 cases. These results suggest that spontaneous regression of herniated intervertebral disc material could occur in affected dogs.”
Steffen F, Kircher PR, Dennler M. Spontaneous regression of lumbar Hansen type 1 disk extrusion detected with magnetic resonance imaging in a dog. J Am Vet Med Assoc. 2014 Mar 15;244(6):715-8. https://pubmed.ncbi.nlm.nih.gov/24568114/
Case description: A 3-year-old French Bulldog was evaluated because of acute signs of back pain and spastic paraparesis.
Clinical findings: Neuroanatomic localization indicated a lesion in the T3-L3 spinal cord segment. Magnetic resonance imaging revealed extradural spinal cord compression at the ventral right aspect of the intervertebral disk space L3-4. On the basis of these findings, a diagnosis of sequestrated Hansen type 1 disk extrusion without extradural hemorrhage was made.
Treatment and outcome: The dog was treated conservatively with cage rest, restricted exercise on a leash, and NSAIDs. Results of follow-up examination 5 weeks later indicated complete resolution of clinical signs, and results of repeated MRI indicated a 69% reduction in the volume of the herniated disk material.
Clinical relevance: Findings for the dog of this report indicated spinal cord compression attributable to extruded intervertebral disk material resolved. Functional improvements in dogs with such problems may be partly attributable to spontaneous regression of intervertebral disk extrusions.
Raimondi F, Moreno-Aguado B, Witte P, Shihab N. Spontaneous resorption of a herniated cervical disc in a dog detected by magnetic resonance imaging. Can Vet J. 2017 Aug;58(8):855-858. https://pubmed.ncbi.nlm.nih.gov/28761194/
This study described the case of a 4-year-old spayed female cocker spaniel dog with a history of neck pain and exercise intolerance. An initial course of gabapentin was administered for 2-weeks with favourable results, but on discontinuance, the neck pain returned. A subsequent MRI confirmed a C3/C4 disc lesion with extruded disc material. Conservative treatment was again administered consisting of crate rest, meloxicam, and gabapentin. Four months later, the dog returned for follow up, with a complete resolution of pain and function. A follow-up MRI was conducted, revealing a resolve of the intervertebral disc herniation. On a telephone follow up 2 years later, the clients reported no recurrence of clinical signs of neck pain.
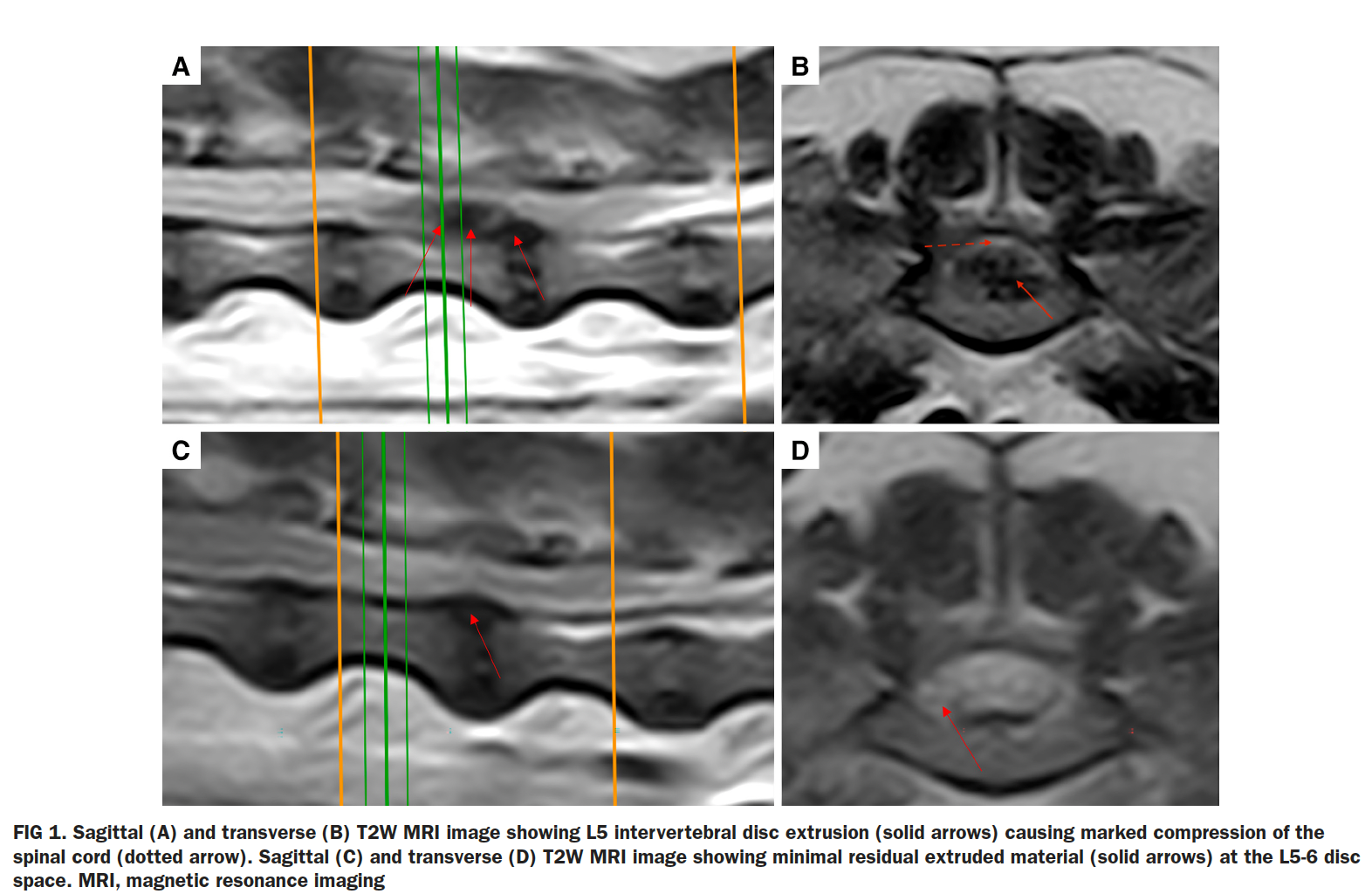
Khan S, Freeman P, Jeffery ND. Spontaneous resolution of severe disc-associated spinal cord compression in a dog. J Small Anim Pract. 2022 Oct;63(10):797. https://pubmed.ncbi.nlm.nih.gov/35729741/
A 7-year-old miniature dachshund was presented with a 4-day history of acute, initially progressive, painful, non-ambulatory paraparesis and urinary incontinence. MRI revealed extruded disc material in the L5 vertebral canal. Due to financial constraints, the dog was managed conservatively with analgesia, cage confinement, bladder expression and physiotherapy. Improvement was rapid with urinary continence regained at 3 days, and the ability to walk 10 steps unaided at 7 days. Twelve weeks later, only mild ambulatory paraparesis persisted with entire spinal reflexes and urinary continence and there was almost complete disappearance of the compressive material on MR images. Mild dorsal bulging of the L5 intervertebral disc persisted.
“The frequency at which spontaneous resolution of disc-associated compression occurs in dogs is unknown, because most affected cases either do not undergo cross-sectional imaging or, alternatively, undergo surgical decompression. In this case, there was rapid improvement in neurologic function, but it is unclear if that was a consequence of spontaneous resolution of compression or arose through purely neurologic recovery mechanisms.”
Freeman P, Jeffery N. Is decompression in acute thoracolumbar intervertebral disc herniation overvalued? Front Vet Sci. 2022 Nov 9;9:1049366. https://pubmed.ncbi.nlm.nih.gov/36439357/
“The general acceptance that surgical decompression is necessary for recovery, especially in dogs that lose deep pain sensation, makes constructing clinical trials of alternative approaches highly problematic. Indeed, in the current opinion environment (25), it would be difficult for any specialist neurologist NOT to recommend decompressive surgery for a non-ambulatory dog with a herniated thoracolumbar disc. So, in view of this ethical background, how can this potentially fallacious dogma be challenged? Several pathways are possible, but an important line of data would be outcomes of dogs that are clear candidates for decompressive surgery according to the current consensus, given their presentation and imaging, but in which this therapy is unavailable because of cost or accessibility. If the outcomes were broadly comparable with those associated with decompressive surgery it would open the path toward randomized controlled trials to compare conservative and surgical therapies, thereby rectifying the current deficiency in formal testing. A greater accumulation of imaging and outcome data following conservative therapy might also aid in suggesting factors associated with poor recovery and allow more rational allocation of animals to surgical or conservative therapy in future.”
Conclusion (mine, that is)
I will continue to assert that conservative management for intervertebral disc herniation should be an option and should include manual therapies (such as mobilizations and traction), modalities (such as photobiomodulation), pharmaceuticals (for control of pain and inflammation), and other adjunct therapies as appropriate (i.e. acupuncture, neuro-rehab techniques to retrain function, UWTM when appropriate, etc.). If such therapies do not yield improvement and/or the condition worsens then most certainly a change in treatment plan (i.e. surgical intervention) would be more appropriate. I abide by the rule of 3: If after three treatments, you are not seeing improvement, then you need to change what you are doing.
If we go back to last week’s blog… I still feel comfortable in using the information presented (albeit human) to recommend mobilizations as part of a conservative management treatment plan for intervertebral disc herniations with the goal of (fingers crossed) disc resorption and/or regression.


