Laurie's Blogs.
Dec 2023
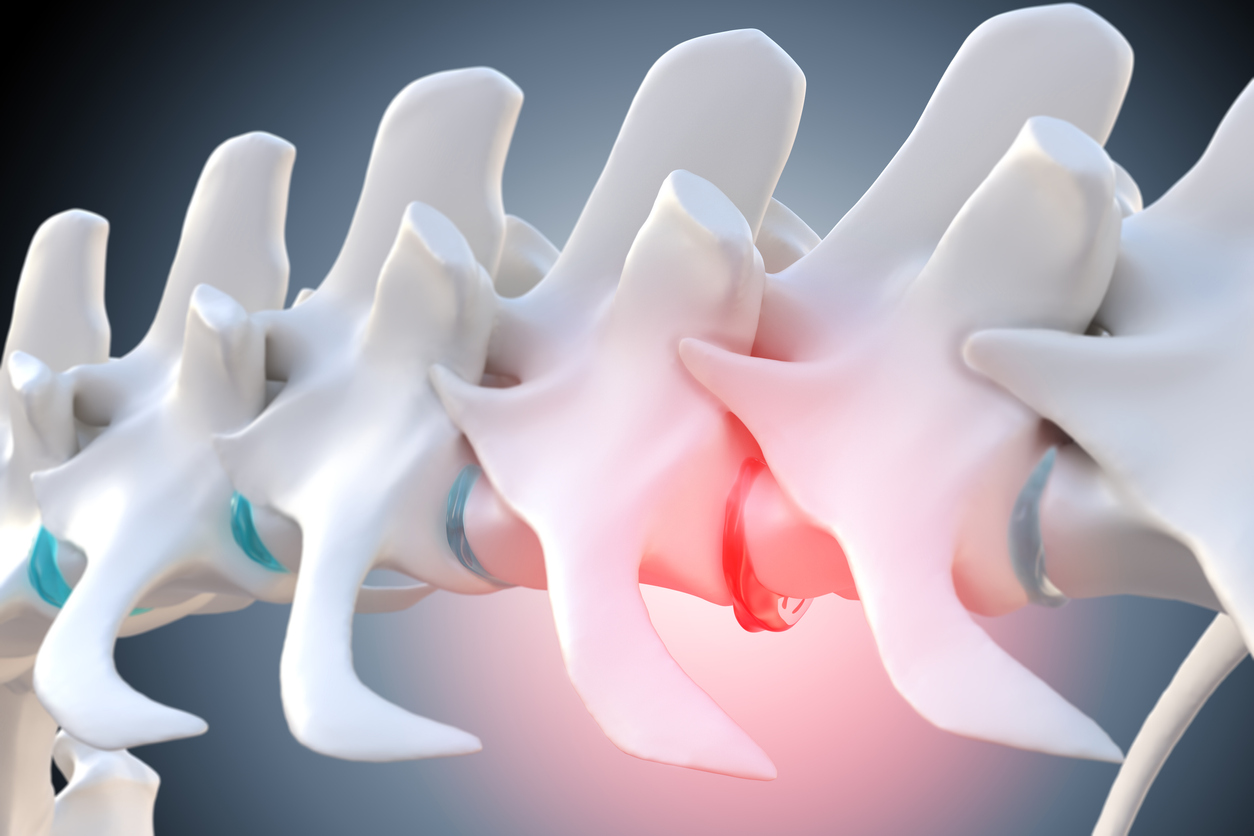
Lumbar Disc Herniations – Mobilize or Manipulate?
A new randomized clinical trial came across my desk - Effects of spinal manipulation or mobilization as an adjunct to neurodynamic mobilization for lumbar disc herniation with radiculopathy: a randomized clinical trial (1). I read it with interest as there always seems to be a debate about which is better – mobilizations or manipulations. Most often, when such studies are done well, the results are that the two interventions yield similar results, and if one understands the neurophysiology behind manual therapy, then that result is understandable.
What is interesting about this study is that it specifically compared the two interventions in regard to a disc herniation with radiculopathy – in other words, lateralized lumbar disc with nerve root compression and subsequent leg pain.
The study took 40 participants with chronic lumbar disc herniations and randomly assigned them into the two groups. Each group also received neurodynamic mobilization (a.k.a. nerve glides, nerve flossing, dural tensioning techniques, neural tensioning techniques…). The spinal manipulation group received a high velocity, low amplitude manipulation and the mobilization group received a Mulligan spinal mobilization with leg movement. (For those unaware, Brian Mulligan was a New Zealand physiotherapist that invented a number of mobilization techniques that incorporated repetitive movements with the mobilizations.) Each group received their treatment regimen twice a week for a span of 12 weeks and were followed and evaluated at the 6-, 12-, 26-, and 52-week mark following randomization.
They were evaluated for back pain, leg pain, activity limitation, sciatica bothersomeness, sciatica frequency, functional mobility, quality of life, and global effect. The primary outcomes were pain and activity limitation at 12 weeks post-randomization.
Findings:
- The results indicate that the MOB group improved significantly better than the SMT group in all outcomes, and at all timelines (6, 12, 26, and 52 weeks post-randomization), except for sensory deficit at 52 weeks, and reflex and motor deficits at 12 and 52 weeks.
- These improvements were also clinically meaningful for neurodynamic testing and sensory deficits at 12 weeks, back pain intensity at 6 weeks, and for activity limitation, functional mobility, and quality of life outcomes at 6, 12, 26, and 52 weeks of follow-ups.
- The risk of being improved at 12 weeks post-randomization was 40% lower in the SMT group compared to the MOB group.
Commentary (mine, that is):
Let’s think about the “why”. When dealing with a disc herniation, the underlying problem is not that a joint isn’t moving properly, and it’s not just a ‘pain’ problem. There is a disc that is bulging, herniated, or extruded. How does a herniated disc improve? It resorbs, it retracts, (or it dehydrates). How best to encourage resorption or retraction? Increasing blood flow. Blood-flow might be better stimulated with repetitive movements (i.e. mobilizations) compared to one isolated event (i.e. manipulation).
In my searching to validate or challenge my ‘why’, I found another very interesting research paper that followed 9 patients with disc hernations all of whom opted for non-surgical interventions. Spontaneous resorption of herniated disk was found in all patients in a mean time of 8.7 ± 3.2 months (2).
“Spontaneous resorption of herniated disk was explained in the literature by 3 common mechanisms. The first mechanism depends on retraction of the herniated disk back to the disk space because it is not separated from the annulus fibrosus. The second mechanism stated that disk resorption is because of dehydration and shrinkage of herniated nucleus pulposus. The third mechanism proposed that the sequestrated nucleus pulposus in the epidural vascular space is recognized by the autoimmune system as a foreign body, which induced an inflammatory reaction resulting in neovascularization, enzymatic degradation, and macrophage phagocytosis of the herniated disk material. The third mechanism was evaluated and supported by different studies.”
It would be important to note, that there are studies that look at spinal manipulation and a reduced incidence of needing spinal surgery in people (3). So, it is not to say that manipulation ‘does not work’, but rather, according to the RCT presented in this blog, mobilization had more favourable results.
Back to the Dogs
I was unable to find any research on canine intervertebral disc herniations and spinal manual therapy treatments. However, and this is a common argument I make, ‘if human medicine utilized foundational animal research to guide clinical treatments for people, why cannot human research be used to guide clinical treatments for animals?’
References
- Danazumi MS, Nuhu JM, Ibrahim SU, et al. Effects of spinal manipulation or mobilization as an adjunct to neurodynamic mobilization for lumbar disc herniation with radiculopathy: a randomized clinical trial. Journal of Manual & Manipulative Therapy, 31:6, 408-420 (2023)
- Elkholy AR, Farid AM, Shamhoot EA. Spontaneous Resorption of Herniated Lumbar Disk: Observational Retrospective Study in 9 Patients. World Neurosurg. 2019 Apr;124:e453-e459.
- Trager RJ, Daniels CJ, Perez JA, Casselberry RM, Dusek JA. Association between chiropractic spinal manipulation and lumbar discectomy in adults with lumbar disc herniation and radiculopathy: retrospective cohort study using United States' data. BMJ Open. 2022 Dec 16;12(12):e068262.


