Laurie's Blogs.
Jun 2023
Alzheimer's Disease: and the Beta-Amyloid Plaque Theory - Update
Sometimes, I just pick a blog topic that I think I want to learn more about. This time, I was curious about Alzheimer’s and the Beta-Amyloid Plaque Theory. I had heard that it had been debunked or challenged, but I hadn’t dove into the research to understand more about this. So, here’s what I found!
Introduction:
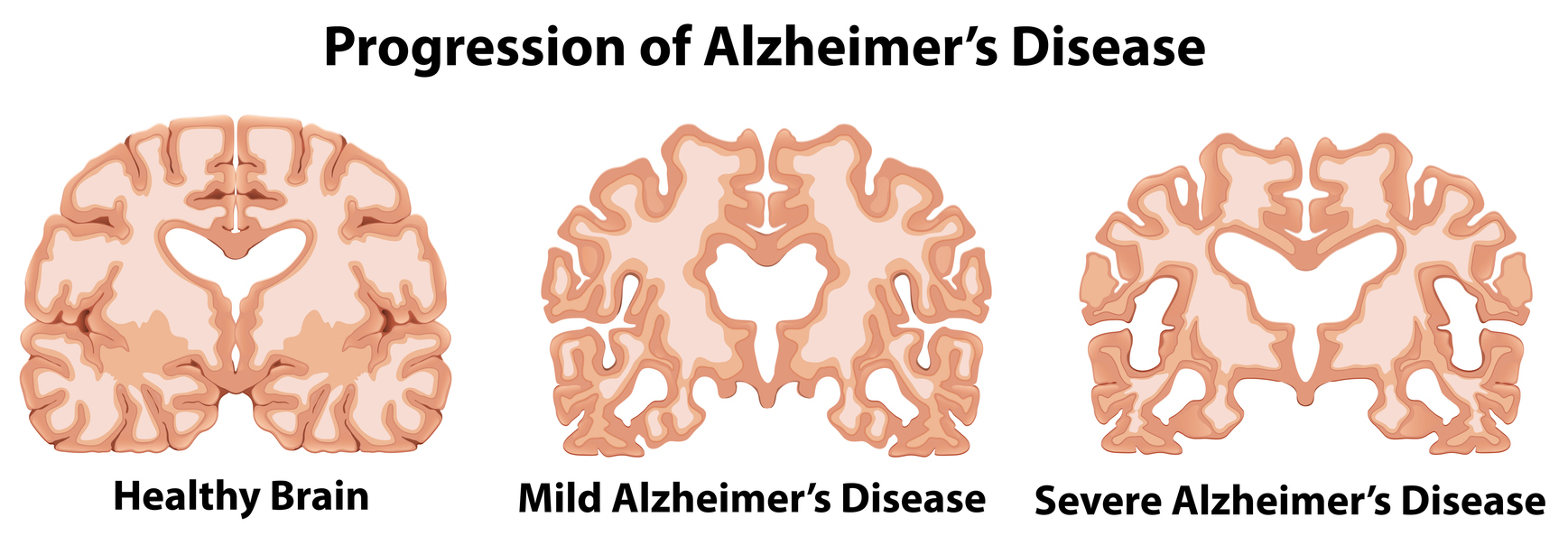
Alzheimer's disease is a debilitating neurodegenerative disorder that affects millions of individuals worldwide. It is recognized that the same condition can affect senior dogs as well, with the name of the condition being termed Canine Cognitive Dysfunction. Over the years, extensive research has been conducted to unravel the underlying mechanisms behind the disease. One prominent feature associated with Alzheimer's is the accumulation of beta-amyloid plaques in the brain. While the amyloid hypothesis has long been the dominant theory explaining the disease's pathology, recent scientific investigations have introduced novel perspectives challenging this traditional view. This blog post aims to explore the latest research and theories surrounding beta-amyloid plaque in Alzheimer's disease.
Beta-Amyloid Plaque: A Historical Perspective
The amyloid hypothesis, proposed in the early 1990s, posits that the accumulation of beta-amyloid plaques is a crucial event triggering Alzheimer's disease. This hypothesis suggests that the aggregated beta-amyloid protein fragments, particularly the amyloid-beta 42 (Aβ42) peptide, cause neurotoxicity, leading to neuronal death and cognitive decline.
Alternative Theories Challenging the Amyloid Hypothesis
2.1. The Prion-Like Spreading Theory:
Emerging evidence suggests that Alzheimer's disease may exhibit prion-like characteristics, where misfolded proteins can propagate and spread throughout the brain. This theory suggests that small aggregates of beta-amyloid or other misfolded proteins act as seeds, inducing the misfolding of normal proteins in adjacent neurons, leading to the formation of new plaques.
2.2. The Clearance Failure Theory:
According to this theory, the accumulation of beta-amyloid plaques in Alzheimer's disease is not solely due to overproduction but is primarily a consequence of impaired clearance mechanisms. Dysfunctional clearance pathways, such as impaired phagocytosis by microglial cells or decreased efficiency of the blood-brain barrier, result in the inadequate removal of beta-amyloid, leading to its accumulation.
2.3. The Oligomerization Hypothesis:
This theory suggests that it is not the mature amyloid plaques themselves but smaller soluble aggregates called oligomers that contribute to neurotoxicity. Oligomers can disrupt synaptic function, induce inflammation, and impair neuronal signaling pathways. They may also trigger the formation of larger plaques and neurofibrillary tangles, exacerbating the disease.
New Approaches Targeting Beta-Amyloid Plaque
Despite the evolving understanding of beta-amyloid plaque, it remains an important target for therapeutic interventions. Several novel strategies are being explored to tackle the accumulation of beta-amyloid in Alzheimer's disease:
3.1. Immunotherapies:
Immunotherapeutic approaches aim to stimulate the immune system to recognize and clear beta-amyloid plaques. Monoclonal antibodies, such as aducanumab, have shown promise in clinical trials by selectively targeting beta-amyloid, facilitating its clearance from the brain.
3.2. Clearance Enhancement:
Enhancing the brain's clearance mechanisms is another avenue of research. Approaches include modulating microglial activity to improve phagocytosis, increasing the permeability of the blood-brain barrier, and developing drugs that promote the degradation and removal of beta-amyloid.
Conclusion
As our understanding of Alzheimer's disease continues to evolve, it is becoming increasingly clear that beta-amyloid plaque plays a complex role in the pathology of the disease. While the amyloid hypothesis has been instrumental in shaping our knowledge, recent theories challenge its exclusivity. The prion-like spreading theory, clearance failure theory, and oligomerization hypothesis offer new perspectives, highlighting the importance of investigating alternative mechanisms.
Moving forward, a comprehensive approach considering multiple factors, including beta-amyloid plaque, neuroinflammation, tau pathology, synaptic dysfunction, and vascular factors, is crucial for a deeper understanding of Alzheimer's disease. Integrating these various aspects will facilitate the development of more effective therapeutic strategies that target the underlying mechanisms of the disease.
It is important to note that while new theories challenging the amyloid hypothesis have gained traction, the field of Alzheimer's research is still evolving. Ongoing studies continue to shed light on the intricate interplay between beta-amyloid plaque and other factors implicated in the disease. By embracing interdisciplinary collaboration and incorporating diverse perspectives, we are poised to make significant strides in the quest to combat Alzheimer's disease.
References:
- Hardy J, Selkoe DJ. The amyloid hypothesis of Alzheimer's disease: progress and problems on the road to therapeutics. Science. 2002;297(5580):353-356. doi: 10.1126/science.1072994
- Morales R, Duran-Aniotz C, Castilla J, Estrada LD, Soto C. De novo induction of amyloid-β deposition in vivo. Mol Psychiatry. 2012;17(12):1347-1353. doi: 10.1038/mp.2011.135
- Sagare AP, Bell RD, Zlokovic BV. Neurovascular dysfunction and faulty amyloid β-peptide clearance in Alzheimer disease. Cold Spring Harb Perspect Med. 2012;2(10):a011452.
- Selkoe DJ. Alzheimer's disease is a synaptic failure. Science. 2002;298(5594):789-791.
- Ferreira ST, Lourenco MV, Oliveira MM, De Felice FG. Soluble amyloid-β oligomers as synaptotoxins leading to cognitive impairment in Alzheimer's disease. Front Cell Neurosci. 2015;9:191.
- Sevigny J, Chiao P, Bussière T, et al. The antibody aducanumab reduces Aβ plaques in Alzheimer's disease. Nature. 2016;537(7618):50-56.
- Salloway S, Sperling R, Fox NC, et al. Two phase 3 trials of bapineuzumab in mild-to-moderate Alzheimer's disease. N Engl J Med. 2014;370(4):322-333.
- Zhang F, Jiang L, Neuroprotective effects of modulation on microglia: potential targets in Alzheimer's disease. Front Aging Neurosci. 2018;10:176.
- Bell RD, Zlokovic BV. Neurovascular mechanisms and blood-brain barrier disorder in Alzheimer's disease. Acta Neuropathol. 2009;118(1):103-113.
- Long JM, Holtzman DM. Alzheimer disease: an update on pathobiology and treatment strategies. Cell. 2019;179(2):312-339.


